About
The intestine and skin constitute surface barriers between the host and the environment, which contains an abundant microbiota, antigens and potential pathogens. As barrier sites are constantly exposed to microbial and damaging elements that may compromise tissue function, a major challenge is to efficiently eliminate pathogens and promote repair while avoiding excessive responses and chronic inflammation. Dysregulation of barrier function leads to several chronic diseases and systemic disorders including inflammatory bowel diseases (IBD), allergic diseases, fibrotic diseases and cancer. Using genetic approaches as well as organoid models, we are investigating the role of the stromal microenvironment in barrier tissues at homeostasis and disease.
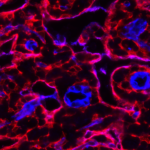
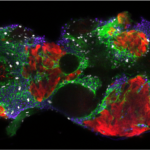
Maintenance of stem cells in adult organs requires a specialized microenvironment called the niche, which provides structural and soluble cues to maintain stemness. In the intestine, maintenance of stem cells requires pro-stemness factors such as Wnt2b produced by peri-cryptal PDGFRalowPdpn+CD34+ stromal cells, while PDGFRaHigh subepithelial stromal cells promote epithelial differentiation by producing bone morphogenetic proteins along the crypt-villus axis. We are interested in the signals that orchestrate spatial and molecular specificities of the intestinal stromal niches. After birth, the intestine undergoes villus and vascular remodeling to fulfill nutrient requirement and enhance intestinal barrier function. We have shown that postnatal PDGFRα-dependent intestinal stromal maturation is required to restrain stemness and promote epithelial differentiation and immunoregulation. Failure of stromal maturation in the first few weeks after birth leads to decreased postnatal growth and dysregulated intestinal inflammatory and repair responses.