Our group is interested in how inflammation regulates mucosal immunity to bacterial infection and cancer in the bladder. By understanding inflammation in this organ, we can target host pathways to manage diseases more effectively to improve patient outcome.
Immunity and improved therapies for UTI
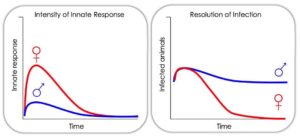 Treatment for urinary tract infection (UTI) relies upon antibiotics, which only treat acute UTI, do not prevent recurrence, and are not efficacious against rapidly disseminating multi-drug resistant (MDR) uropathogenic E. coli (UPEC). We are identifying novel ways to target host pathways to treat UTI that do not depend upon antibiotics. Our work supports that the innate response shapes the nature of the long-term adaptive response to UTI. We examine how sex (i.e., being female or male), resident immune cells, and innate immune pathways influence development of long-lasting immunity to UTI. In addition, focusing on three non-antibiotic based therapies approved for use in humans in other contexts, we are testing how manipulating the innate host response may improve outcomes and reduce recurrent infection.
Treatment for urinary tract infection (UTI) relies upon antibiotics, which only treat acute UTI, do not prevent recurrence, and are not efficacious against rapidly disseminating multi-drug resistant (MDR) uropathogenic E. coli (UPEC). We are identifying novel ways to target host pathways to treat UTI that do not depend upon antibiotics. Our work supports that the innate response shapes the nature of the long-term adaptive response to UTI. We examine how sex (i.e., being female or male), resident immune cells, and innate immune pathways influence development of long-lasting immunity to UTI. In addition, focusing on three non-antibiotic based therapies approved for use in humans in other contexts, we are testing how manipulating the innate host response may improve outcomes and reduce recurrent infection.
Novel immunotherapy for bladder cancer
Bacillus Calmette-Guérin (BCG) instillation is the standard-of-care for nonmuscle invasive 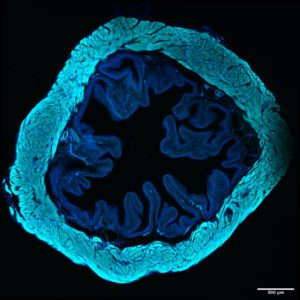 bladder cancer, the fifth most common malignancy in Europe and the U.S and is one of the most successful immunotherapies in use today. Nonetheless, 30-50% of patients fail to respond to BCG immunotherapy and models to understand this are lacking. We developed novel bladder cancer models in which mechanisms of action of known and new mono and combination immunotherapy can be dissected, and T cell priming and effector function can be directly followed. We aim to improve T cell function to improve tumor immunity. With this knowledge, we can rationally design combination immunotherapeutic approaches to reduce the incidence of BCG unresponsiveness or tumor recurrence, establishing alternatives to surgical resection and chemotherapy, for improved patient outcomes. Micrograph: Livia Lacerda Mariano
bladder cancer, the fifth most common malignancy in Europe and the U.S and is one of the most successful immunotherapies in use today. Nonetheless, 30-50% of patients fail to respond to BCG immunotherapy and models to understand this are lacking. We developed novel bladder cancer models in which mechanisms of action of known and new mono and combination immunotherapy can be dissected, and T cell priming and effector function can be directly followed. We aim to improve T cell function to improve tumor immunity. With this knowledge, we can rationally design combination immunotherapeutic approaches to reduce the incidence of BCG unresponsiveness or tumor recurrence, establishing alternatives to surgical resection and chemotherapy, for improved patient outcomes. Micrograph: Livia Lacerda Mariano