Link to Pubmed [PMID] – 35157765
Link to HAL – pasteur-03599568
Link to DOI – 10.1182/blood.2021014654
Blood 2022 Apr; 139(17): 2585-2600
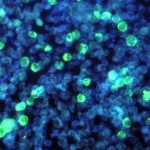
Both innate and adaptive lymphocytes have critical roles in mucosal defense that contain commensal microbial communities and protect against pathogen invasion. Here we characterize mucosal immunity in patients with severe combined immunodeficiency (SCID) receiving hematopoietic stem cell transplantation (HSCT) with or without myeloablation. We confirmed that pretransplant conditioning had an impact on innate (natural killer and innate lymphoid cells) and adaptive (B and T cells) lymphocyte reconstitution in these patients with SCID and now show that this further extends to generation of T helper 2 and type 2 cytotoxic T cells. Using an integrated approach to assess nasopharyngeal immunity, we identified a local mucosal defect in type 2 cytokines, mucus production, and a selective local immunoglobulin A (IgA) deficiency in HSCT-treated SCID patients with genetic defects in IL2RG/GC or JAK3. These patients have a reduction in IgA-coated nasopharyngeal bacteria and exhibit microbial dysbiosis with increased pathobiont carriage. Interestingly, intravenous immunoglobulin replacement therapy can partially normalize nasopharyngeal immunoglobulin profiles and restore microbial communities in GC/JAK3 patients. Together, our results suggest a potential nonredundant role for type 2 immunity and/or of local IgA antibody production in the maintenance of nasopharyngeal microbial homeostasis and mucosal barrier function.