About
Quique BASSAT – Barcelona Institute of Global health ISGlobal (Barcelone – Espagne)
In spite of large efforts and generous investments, mortality statistics and cause of death (CoD) estimates from resource-constrained countries remain, as of 2016, still unreliable. Models utilized to build estimates for poor countries, where the majority of preventable deaths still occur, have shown many flaws, and discrepancies in cause-attributable disease figures have evidenced the shortfall of current methods, predominantly based in data derived from verbal autopsy or clinical records. With efforts targeting the improvement of civil and vital registration systems (CVRS), counting the dead has become progressively easier, but establishing the cause of every single one of those deaths remains a major challenge. Routine and cause-specific disaggregated mortality data are however critical at the local level to help policy makers adequately tailor health planning and prioritisation.
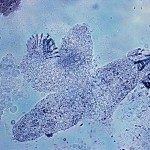
In this context, the CaDMIA (Cause of Death using Minimally invasive autopsies) consortium was established in the year 2012, with funding from the Bill and Melinda Gates Foundation, with the objective of validating a novel post-mortem approach that could improve the CoD attribution in settings where robust CoD data are most needed, but where the feasibility of conducting post-mortem evaluations is lowest. Pathological autopsies are generally considered the gold standard methodology to investigate CoD, but their practice is globally decreasing, and in the majority of poor settings their routine use and acceptability is severely limited. The consortium aimed at comparing the performance of a minimally invasive autopsy (MIA) protocol approach, where fine biopsy needles would be used to obtain tissues and fluids from key organs, with that of the complete diagnostic autopsy (CDA). In parallel, the consortium aimed at establishing the hypothetical feasibility and acceptability of this new approach, under the hypothesis that a less disfiguring and specialised method could be found more readily acceptable and implementable in rural and poor settings. Coordinated from the Barcelona Institute of Global health (ISGlobal), in Spain, the consortium included partners in four African countries (Mozambique, Gabon, Kenya and Mali), the Brazilian Amazon and Pakistan.
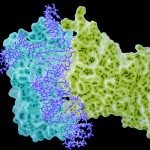
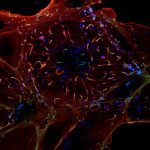
In this talk, I would like to share the results of the validation exercise of the MIA method, and its theoretical acceptability and feasibility as explored during the project in a wide variety of settings. In addition, I would also like to highlight some of the pre-mortem research of our group, particularly on the areas of innovation for diagnosis of malaria, pneumonia, and meningitis.
Contact : Chetan Chitnis (chetan.chitnis@pasteur.fr – Poste : 9428)