Présentation
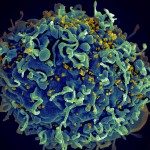
Broadly neutralizing HIV-1 antibodies (bNAbs) can develop in rare infected individuals several years after co-evolution with diversifying viruses. In animal models, passive immunotherapy with potent HIV-1 bNAbs has been shown to protect from infection and importantly, to substantially reduce viraemia in infected humans.
Immunoprophylaxis with potent bNAbs efficiently protects non-human primates from mucosal transmission even after repeated challenges. However, the precise mechanisms of bNAbs-mediated viral inhibition in mucosal tissues were still unexplored. Our work showed that bNAbs, produced as recombinant IgG but also IgA mAbs (Lorin et al, 2015), did not interfere with the endocytic transport of HIV-1 across epithelial cells, a process referred to as transcytosis. Instead, both free and antibody-opsonized virions were translocated to the basal pole of epithelial cells. Importantly, as opposed to free viruses, viral particles bound by bNAbs were no longer infectious after transepithelial transit. Post-transcytosis neutralization activity of bNAbs displayed comparable inhibitory concentrations as those measured in classical neutralization assays. Overall, our results show that bNAbs do not block the transport of incoming HIV-1 viruses across the mucosal epithelium but rather neutralize the transcytosed virions, highlighting their efficient prophylactic and protective activity in vivo (Lorin et al, 2017).
HIV-1 can cross the blood-brain barrier (BBB) to penetrate the brain and infect target cells, causing neurocognitive disorders as a result of neuroinflammation and brain damage. The HIV-1 envelope spike gp160 is partially required for viral transcytosis across the BBB endothelium. But do antibodies developing in infected individuals and targeting the HIV-1 gp160 glycoproteins block HIV-1 transcytosis through the BBB? We addressed this issue and discovered that anti-gp160 antibodies do not block HIV-1 transport; instead, free viruses and those in complex with antibodies can transit across BBB endothelial cells. Importantly, we found that only neutralizing antibodies could inhibit post-transcytosis viral infectivity, highlighting their ability to protect susceptible brain cells from HIV-1 infection (Lorin et al, 2020).
Human high affinity antibodies to pathogens often recognize unrelated ligands. The molecular origin and the role of this polyreactivity are largely unknown. Several unusual but essential immunoglobulin features characterize HIV-1 bNAbs, some of which are associated with antibody polyreactivity. To better appreciate whether polyreactivity contributes to HIV-1 neutralization or simply be a bystander effect of affinity maturation, we aimed at elucidating the molecular mechanisms linking acquisition of bNAbs activity with poly- / auto-reactivity. We found that HIV-1 bNAbs were frequently polyreactive, cross-reacting with non-HIV-1 molecules including self-antigens. Mutating bNAb genes to increase HIV-1 binding and neutralization also created de novo polyreactivity. Using binding affinity, thermodynamic and molecular dynamics analyses, we showed that unliganded paratopes of polyreactive bNAbs with improved HIV-1 neutralization exhibited a conformational flexibility. Hence, promiscuous reactivity of HIV-1 bNAbs can be inputted to the binding sites’ flexibility, triggered by somatic hypermutations, which aid in accommodating not only divergent HIV-1 Env glycoproteins but also topologically distinct non-HIV-1 molecules via plastic hydrophobic structural interfaces (Prigent et al, 2018). This suggests that affinity maturation of HIV-1-reactive B cells towards neutralizing breadth may be tightly regulated between the selection of clones with “adaptable” antibody binding sites for an expanded HIV-1 recognition and the counterselection by immune tolerance of highly polyreactive clones reacting with self-antigens. We speculate that this phenomenon may occur with other pathogens with diversifying antigens, making antibodies’ natural development or elicitation by vaccines particularly difficult.
Apart from neutralization, the Fc region of HIV-1 bNAbs is required for suppressing viremia, through mechanisms that remained poorly understood. In a collaborative work with the team led by Olivier Schwartz (Institut Pasteur), we aimed at identifying HIV-1 bNAbs that exert ADCC in cell culture and kill HIV-1-infected lymphocytes through NK engagement. We found that: (i) most bNAbs were potent ADCC-mediators; (ii) the landscape of gp160 epitope exposure at the surface and the sensitivity of infected cells to ADCC varied considerably between viral strains; (iii) efficient ADCC required sustained cell surface binding of bNAbs to gp160; (iv) reactivated infected cells from HIV-positive individuals exposed heterogeneous envelope protein levels that are often sufficient to trigger killing by bNAbs or bNAb mixtures. Thus, this study allowed delineating the parameters controlling ADCC activity of bNAbs, and supports the use of the most potent bNAbs to clear the viral reservoir (Bruel et al, 2016). In a follow-up work, non-neutralizing antibodies (nnAbs) and bNAbs’ potencies to bind and eliminate HIV-1-infected cells in culture were compared. Overall, data revealed important qualitative and quantitative differences between nnAbs and bNAbs in their ADCC capacity and strongly suggest that the breadth of recognition of HIV-1 by nnAbs is narrow (Bruel et al, 2017). More recently, the Schwartz lab in collaboration with our group showed that HIV-1 bNAbs, can triggers C3 deposition and complement-dependent cytotoxicity (CDC) on Env-expressing Raji cells. Primary CD4 T cells infected with laboratory-adapted or primary HIV-1 strains and treated with bNAbs are susceptible to C3 deposition but not to rapid CDC. The cellular protein CD59 and viral proteins Vpu and Nef protect infected cells from CDC mediated by bNAbs or by polyclonal IgGs from HIV-positive individuals. However, complement deposition accelerates the disappearance of infected cells within a few days of culture. Altogether, these results uncovered the contribution of complement to the antiviral activity of anti-HIV-1 bNAbs (Dufloo et al, 2020).