About
Hepatocellular carcinoma is the principal form of primary liver cancer, the fifth most common human cancer (with 800000 new cases every year) and the 2nd cause of mortality by cancer worldwide. Hepatocellular carcinoma affects usually patients in their maturity albeit with substantial variations depending on the continent considered (eg 5th decade of life in Africa, 7th in Europe). Hepatitis viruses (B and C), alcohol abuse, mycotoxins and some metabolic diseases represent the most important risk factors of hepatocellular carcinoma.
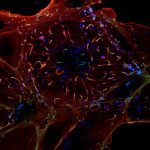
Hepatocellular carcinoma from young Peruvian patients
We identified in Peru an unusual form of hepatocellular carcinoma with a unique clinical presentation, as it affects patients around age 25 and represents half of the novel cases attending care at the National Institute for Tumor Diseases of Lima (INEN). In collaboration with INEN (Dr E. Ruiz) and the Institut de Recherches pour le Développement (IRD, Drs S. Bertani and E. Deharo), we decided to decipher the molecular processes explaining this unusual presentation. To this aim, we follow a multimodal integrative approach targeting genomic, epigenomic, transcriptomic and viral features. The working hypothesis is that this juvenile form of hepatocellular carcinoma is associated with a particular molecular defect that accelerates the kinetics of tumor development in affected individuals. On a longer term, the secondary objective of our research is to look for a similar or connected defect in young patients (children, adolescents, young adults) developing a carcinoma of any tissue origin in other places of the world.
Our preliminary results indicate that hepatitis B virus (HBV) DNA is found in 80% of liver tissues with younger patients harboring significantly higher virus loads than elder. Furthermore, different types of mutations affecting viral DNA were observed in young or elder individuals suggesting that HBV restriction process is different in each category of patients. We noticed thereafter that various DNA repair proteins, potentially responsible of the observed mutations are differentially expressed in young and elder patients. In parallel, oncogenes and onco-suppressors mutation spectra analysis was carried out on several mutation hostpsots revealing unique features such as a major class of alterations represented by insertions/deletions, a situation suggesting, here again, a significant defect in DNA repair. transcriptome/methylome analyses are currently ongoing to further characterize main pathways altered in young peruvian patients.
Detection of free circulating DNA mutations in hepatocellular carcinoma
Hepatocellular carcinoma is a deadly disease and to benefit from curative surgery, patients should be diagnosed early. Unfortunately, because the lack of biomarkers usable to routinely screen patients at-risk of hepatocellular carcinoma, a vast majority of them are not treated by surgery. Free circulating tumor DNA (fcDNA) is currently considered as a promising material (“liquid biopsy”) to detect early tumors or cancer relapse in different tumor types. The aim of our research program is to develop from fcDNA a panel of sensitive markers increasing the proportion of patients with hepatocellular carcinoma detected at an early stage. Patients have been recruited in a joint program with Centre Pasteur du Cameroun in Yaoundé (Dr Richard Njouom) and the Institut Pasteur of Bangui in Central African Republic (CAR, Dr Claudine Bekondi) working in close collaboration with local hospitals (Hôpital Central and Hôpital de l’Amitié, respectively).
We set out to detect point mutations, chromosome copy number variation and aberrant methylation on fcDNA using the most sensitive techniques of amplification available. We are currently testing a series of DNA extracted from patients with and without hepatocellular carcinoma. In parallel, high-throughput sequencing techniques were applied both on DNA from tumor biopsies and fcDNA to detect novel putative African patients-specific mutations. Preliminary results reveal a great consistence of mutation rates in hepatocellular carcinoma patients from Cameroon (42%) and CAR (29%). In addition, patients with chronic liver diseases were also carrying alterations suggesting that mutational process affecting the patients begins, in reality, well before tumor apparition and is easily detectable in the blood. Prospective studies are now warranted to determine whether DNA mutants could predict tumor apparition in individual without tumors at enrollment.