Lien vers Pubmed [PMID] – 40617588
Lien DOI – 10.1136/rmdopen-2025-005673
RMD Open 2025 Jul; 11(3):
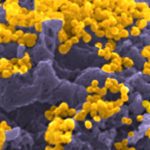
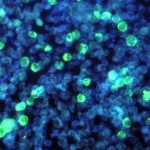
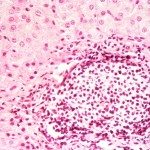
Patients with rheumatoid arthritis (RA) and spondyloarthritis (SpA) are at an increased risk for infection related to the use of immunomodulatory therapies (ITs). The objective of this study is to assess the impact of ITs on the adaptive immune responses to SARS-CoV-2.The study population comprised 94 patients (48 SpA; 46 RA; mean age of 53±14 years) with a confirmed SARS-CoV-2 infection. 20 age-matched individuals (50±17 years), corresponding to the patients’ household contacts infected at the same time, were included as the control population. Patients were stratified by treatment groups: methotrexate (MTX)/sulfasalazine (n=17/2), anti-TNF (n=24), anti-TNF+MTX (n=23), RTX (N=11), anti-IL17 (n=7) and others (n=11). The study compared the viral loads in plasma, stools and nasal swabs and the SARS-CoV-2-specific humoral and cellular immune responses (antibodies, B and T lymphocytes) following SARS-CoV-2 infection.Viral persistence was not observed in the blood, nasopharynx and stools of patients undergoing ITs. Overall, the SARS-CoV-2-specific humoral and T-cell responses were preserved. Patients receiving RTX showed significantly lower IgA and IgG responses to SARS-CoV-2 compared with other treatment groups. Most patients, including RTX recipients, exhibited significant CD4+T cell responses. However, RTX therapy was associated with reduced SARS-CoV-2-specific activated CD8+T cells. A correlation was observed between humoral immune parameters and CD8+ T cell activation.While most patients demonstrated the capacity to mount an immune response to SARS-CoV-2, treatment with RTX impacted both humoral and CD8+cell responses. Developing vaccines that elicit robust CD8+T cell responses could offer benefits to individuals undergoing ITs for inflammatory rheumatic diseases.