Link to Pubmed [PMID] – 22329526
Link to DOI – 10.1111/j.1469-0691.2012.03764.x
Clin Microbiol Infect 2012 Apr; 18(4): E99-E109
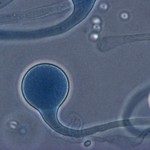
Limited data exist on Candida endocarditis (CE) outcome in the era of new antifungals. As early diagnosis of CE remains difficult, non-culture-based tools need to be evaluated. Through the French prospective MYCENDO study (2005-2007), the overall characteristics and risk factors for death from CE were analysed. The contribution of antigen detection (mannan/anti-mannan antibodies and (1,3)-β-d-glucans) and molecular tools was evaluated. Among 30 CE cases, 19 were caused by non-albicans species. Sixteen patients (53%) had a predisposing cardiac disease, which was a valvular prosthesis in ten (33%). Nine patients (30%) were intravenous drug users; none of them had right-sided CE. Among the 21 patients who were not intravenous drug users, 18 (86%) had healthcare-associated CE. Initial therapy consisted of a combination of antifungals in 12 of 30 patients (40%). Thirteen patients (43%) underwent valve replacement. The median follow-up was 1 year after discharge from hospital (range, 5 months to 4 years) and hospital mortality was 37%. On univariate analysis, patients aged ≥60 years had a higher mortality risk (OR 11, 95% CI 1.2-103.9; p 0.024), whereas intravenous drug use was associated with a lower risk of death (OR 0.12, 95% CI 0.02-0.7; p 0.03). Among 18 patients screened for both serum mannan/anti-mannan antibodies and (1,3)-β-d-glucans, all had a positive result with at least one of either test at CE diagnosis. Real-time PCR was performed on blood (SeptiFast) in 12 of 18, and this confirmed the blood culture results. In conclusion, CE prognosis remains poor, with a better outcome among younger patients and intravenous drug users. Detection of serum antigens and molecular tools may contribute to earlier CE diagnosis.