Link to Pubmed [PMID] – 31292264
Link to DOI – eaat147910.1126/scitranslmed.aat1479
Sci Transl Med 2019 Jul; 11(500):
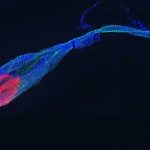
Anaphylaxis is a systemic acute hypersensitivity reaction that is considered to depend on allergen-specific immunoglobulin E (IgE) antibodies and histamine release by mast cells and basophils. Nevertheless, allergen-specific IgG antibodies have been proposed to contribute when the allergen is an abundant circulating large molecule, e.g., after infusions of therapeutic antibodies or dextran. Data from animal models demonstrate a pathway involving platelet-activating factor (PAF) release by monocytes/macrophages and neutrophils activated via their Fc gamma receptors (FcγRs). We hypothesized that such a pathway may also apply to small drugs and could be responsible for non-IgE-mediated anaphylaxis and influence anaphylaxis severity in humans. We prospectively conducted a multicentric study of 86 patients with suspected anaphylaxis to neuromuscular-blocking agents (NMBAs) during general anesthesia and 86 matched controls. We found that concentrations of anti-NMBA IgG and markers of FcγR activation, PAF release, and neutrophil activation correlated with anaphylaxis severity. Neutrophils underwent degranulation and NETosis early after anaphylaxis onset, and plasma-purified anti-NMBA IgG triggered neutrophil activation ex vivo in the presence of NMBA. Neutrophil activation could also be observed in patients lacking evidence of classical IgE-dependent anaphylaxis. This study supports the existence of an IgG-neutrophil pathway in human NMBA-induced anaphylaxis, which may aggravate anaphylaxis in combination with the IgE pathway or underlie anaphylaxis in the absence of specific IgE. These results reconcile clinical and experimental data on the role of antibody classes in anaphylaxis and could inform diagnostic approaches to NMBA-induced acute hypersensitivity reactions.