About
HBV infection can be successfully controlled by natural immune responses in more than 90% of the patients infected as adults, and in the ~1% of chronically infected patients who spontaneously clear the infection (also called HBV seroconverters), as defined by HBs antigen loss and anti-HBs antibody seroconversion.
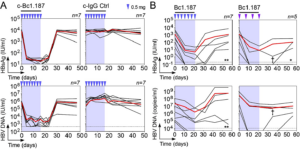
To better understand the memory B-cell immunity to HBV and identify cross-neutralizing epitopes on the HBS surface antigen (HBsAg), we single-cell FACS captured HBsAg-specific memory B cells from HBV vaccinees and seroconverters, cloned and characterized 73 anti-HBV mAbs. We found that most HBV-specific memory B cells: (i) displayed a biased immunoglobulin repertoire; (ii) expressed surface IgG recognizing conformational epitopes; (iii) cross-reacted against various HBV genotypes and naturally-occurring escape mutants. Importantly, 61% of the HBV mAbs neutralized HBV infection in vitro and among those, half were extremely potent (IC50s ~ pg/ml). Finally, we identified at least six non-overlapping neutralizing epitopes on HBsAg. Using two different mouse models of HBV infection, we demonstrated that immunotherapy with a potent HBV bNAb, Bc1.187, can suppress viraemia in vivo. Altogether, our data indicate that the memory B-cell response to HBsAg in HBV vaccinees and seroconverters is diverse in terms of gene repertoire, targeted epitopes and neutralizing activity. Thus, human neutralizing HBsAg antibodies appear to play a key role in the spontaneous control of HBV and represent promising immunotherapeutic tools for achieving a functional cure in chronic HBV carriers. | Hehle*, Beretta* et al, J Exp Med 2020 |.
Figure. Therapeutic activity of HBV bNAb Bc1.187 in HBV-carrier (A) and HBV-infected humanized liver (B) mouse models. n: number of mice. The red line indicates the average.