Methicillin-resistant staphylococcus aureus (MRSA) is a major focus for infection control effort globally. The migration of community-acquired-MRSA (CA-MRSA) into hospitals and the recent increasing antibiotic resistance of CA-MRSA strains make this pathogen difficult to treat because of the presence of a broad array of virulence factors and genomic plasticity. Biofilm formation is a mechanism that contributes to the pathogenesis of S. aureus in infected cutaneous wounds by conferring protection against antibiotics and host immune response. The versatility of S. aureus to form biofilm is central to the pathology of difficult-to-treat skin injuries, including burns caused by heat. As part of our research project, we are developing understanding about mechanisms involved in biofilm formation and how it shapes pathological S. aureus wound infection. We aim to develop new treatments that provide antibacterial and anti-biofilm activity at the source of the infection. An ideal antimicrobial treatment should effectively reduce bacterial wound burden without compromising viability of the host cells. It should safely promote rapid healing with optimal functional and aesthetically pleasing outcomes.
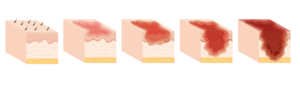
Cutaneous wounds