About
Perinatal HIV infection – ANRS-EP38-IMMIP
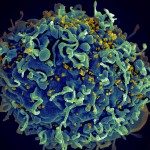
Potent combined antiretroviral therapy has transformed HIV disease into a stable chronic condition. Infected children born at the beginning of the epidemic are now reaching adulthood. The unique characteristics of perinatal infection described in children may be altered by long-term exposure to viral replication, various antiretroviral treatments and puberty. In 2007, we set up a collaborative study to study such patients with 10 clinical sites and the ANRS-CO-10 cohort that follows infected children since birth.
Our hypothesis was that the specificity of the period of infection and the whole disease history influence the following four immune mechanisms and their evolution under potent therapy: thymic activity that is a crucial factor for the immune response to new infections and vaccines; premature ageing of the immune system; immune activation; and HIV-specific T lymphocytes that control viral replication. The aim of the study was to characterise these immune parameters in perinatally infected subjects as they reach adulthood and to assess their association with current and past HIV disease, which is known since birth for these patients.
The 93 patients included were between 15 and 24 years of age at the time of the study. Seventy-nine (85%) patients were receiving cART and plasma HIV RNA was undetectable in 75% of the treated patients. Most patients had reached advanced stages of disease: 80% had had at least one CD4 cell percentage below 15% and only four of them had never received HAART.
The major result of this work was that naive CD4 T lymphocytes were present in proportion similar to those of uninfected young adults. Furthermore, neither naive CD4 T lymphocytes levels, nor the proportion of recent thymic emigrants were reduced in patients with viral replication. The level of total HIV DNA in PBMCs, which reflects the size of the viral reservoir, was associated with viral replication over the last 10 years. In contrast to reports in adults, the HIV DNA level was not associated with CD4 T cell counts.