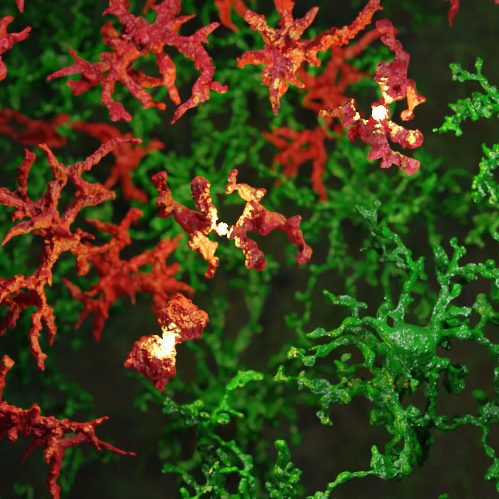
The brain has its own resident immune cells, microglia, that perform maintenance in the normal brain and provide an immune response to injury or infection. Bone marrow transplantation is a regularly used clinical procedure with over 50,000 transplantations worldwide each year. After transplantation these brain microglia are gradually replaced with bone marrow-derived immune cells, macrophages, yet, the mechanism how this transfer of cells was largely unknown.
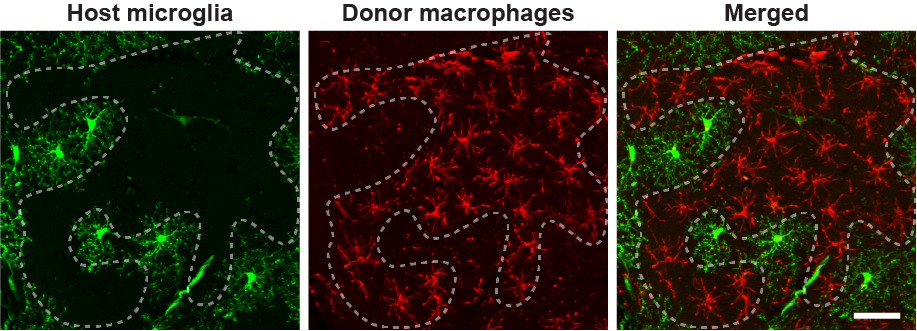
Sailor and colleagues of the unit Perception and Memory, along with collaborators at the Paris Brain Institute published their study in Nature Medicine unmasking the mechanism of macrophage engraftment. Using a mouse model, they showed the chemotherapy agent used in bone marrow transplantation, busulfan, to cause microglia to be incapable of cell division, becoming senescent, which drove their replacement with macrophages derived from the donor cell bone marrow stem cells. They also performed in vivo imaging over multiple months, tracking individual macrophages, showing them to become resident in the brain with similar dynamics of their processes, potentially fulfilling the role of the microglia they replaced. These findings are important since the prevalence of this clinical procedure and to understand how it is used to treat various white matter diseases while helping to find the cause of off-target effects for transplant survivors.
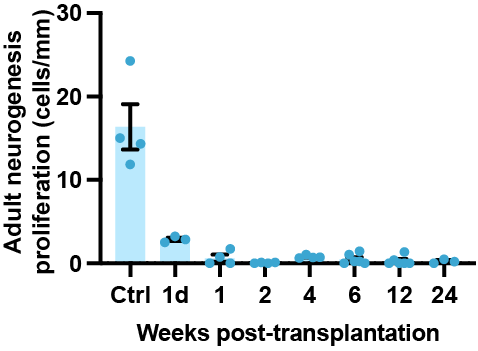
“The chemo-brain”, a widely observed side effect of chemotherapy includes distinct memory and learning impairments. In this study, the authors found that within a few days after busulfan chemotherapy all adult neurogenesis was ablated. Adult neurogenesis is a processes where new neurons are continually being created in specific regions of the adult brain and it is thought to be important for learning and memory functions. Thus its loss after busulfan chemotherapy could cause these cognitive side-effects, yet further human-specific research is needed.
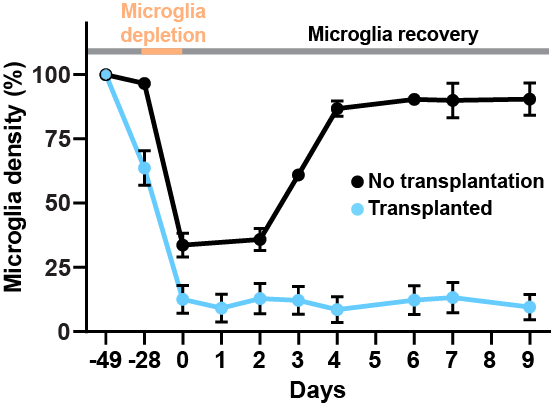
In the normal brain, studies showed administering a drug that almost completely depopulates microglia which was followed by drug withdrawal caused brain microglia to undergo massive cell proliferation and repopulate the entire brain, without any peripheral macrophages undergoing engraftment. In this study the authors performed the same experiment in the post-transplanted brain and showed a complete loss of regenerative capacity of microglia, with the subsequent near-complete replacement of the brain with donor macrophages.
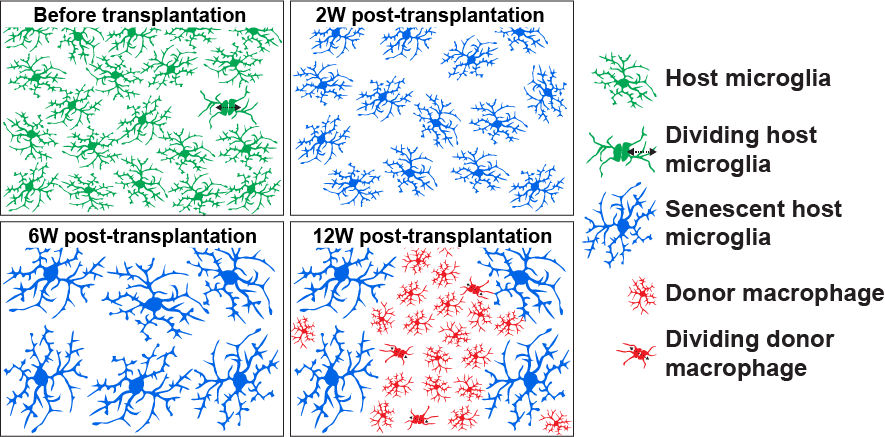
Interestingly, busulfan chemotherapy is used prior to bone marrow transplantation for depleting host bone marrow stem cells to provide an empty niche for donor stem cells to engraft in the bone marrow, thereby replacing the host stem cell population. The authors propose a similar mechanism in the brain, with the gradual depletion of microglia, coupled with their loss of regenerative capacity, providing an empty niche in the brain for donor macrophages, albeit at a much slower pace than with bone marrow cells. Taken together, this study provides a mechanism that could be further enhanced to increase brain macrophage transplantation efficiency and to find new methods of transplantation that avoid the side effects of current chemotherapy agents.
Source:
Research briefing: Bone marrow transplantation chemotherapy disrupts regenerative brain cell populations. Nat Med (2022). https://doi.org/10.1038/s41591-022-01722-5