Link to Pubmed [PMID] – 36135376
Link to DOI – e02874-2210.1128/spectrum.02874-22
Microbiol Spectr 2022 Oct; 10(5): e0287422
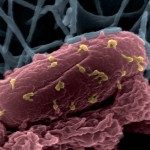
Bacteria developing resistance compromise the efficacy of antibiotics or bacteriophages (phages). We tested the association of these two antibacterials to circumvent resistance. With the Hollow Fiber Infection Model (HFIM), we mimicked the concentration profile of ciprofloxacin in the lungs of patients treated orally for Pseudomonas aeruginosa infections and, independently, mimicked a single inhaled administration of phages (one or two phages). Each treatment selects for antibiotic- or phage-resistant clones in less than 30 h. In contrast, no bacteria were recovered from the HFIM at 72 h when ciprofloxacin was started 4 h post phage administration, even when increasing the initial bacterial concentration by 1,000-fold. The combination of phages with antibiotics used according to clinical regimens prevents the growth of resistant clones, providing opportunities to downscale the use of multiple antibiotics. IMPORTANCE In the treatment of bacterial infections, the use of antibiotics or bacteriophages (phages) is limited by the ability of bacteria to develop resistance. The resistance frequency depends on the exposure to antibacterials. Therefore, determination of concentration profiles of antibiotics is key to define optimal regimens during treatments. In the laboratory, the Hollow Fiber Infection Model (HFIM) mimics concentration profiles observed in patients. In this study, we used the HFIM to evaluate the killing efficacy of the combination of phages and ciprofloxacin. We demonstrated that dosing schedule of phages first and the antibiotic second prevent the selection of resistant bacteria. These results demonstrate that combination efficacy relies on a strong initial reduction of the bacterial population by phages followed by antibiotics before any resistant arise.