Link to Pubmed [PMID] – 17331978
Hum. Mol. Genet. 2007 Apr;16(8):982-92
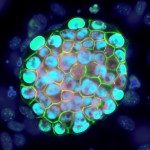
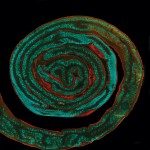
Cerebral Autosomal Dominant Arteriopathy with Subcortical infarcts and Leukoencephalopathy (CADASIL) is the most prominent known cause of inherited stroke and vascular dementia in human adult. The disease gene, NOTCH3, encodes a transmembrane receptor primarily expressed in arterial smooth muscle cells (SMC). Pathogenic mutations lead to an odd number of cysteine residues within the NOTCH3 extracellular domain (NOTCH3(ECD)), and are associated with progressive accumulation of NOTCH3(ECD) at the SMC plasma membrane. The murine homolog, Notch3, is dispensable for viability but required post-natally for the elaboration and maintenance of arteries. How CADASIL-associated mutations impact NOTCH3 function remains a fundamental, yet unresolved issue. Particularly, whether NOTCH3(ECD) accumulation may titrate the ligand and inhibit the normal pathway is unknown. Herein, using genetic analyses in the mouse, we assessed the functional significance of an archetypal CADASIL-associated mutation (R90C), in vivo, in brain arteries. We show that transgenic mouse lines expressing either the wild-type human NOTCH3 or the mutant R90C human NOTCH3, at comparable and physiological levels, can rescue the arterial defects of Notch3-/- mice to similar degrees. In vivo assessment of NOTCH3/RBP-Jk activity provides evidence that the mutant NOTCH3 protein exhibits normal level of activity in brain arteries. Remarkably, the mutant NOTCH3 protein remains functional and does not exhibit dominant negative interfering activity, even when NOTCH3(ECD) accumulates. Collectively, these data suggest a model that invokes novel pathogenic roles for the mutant NOTCH3 protein rather than compromised NOTCH3 function as the primary determinant of the CADASIL arteriopathy.