Link to Pubmed [PMID] – 30911587
Mol Ther Methods Clin Dev 2019 Jun;13:303-309
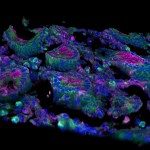
Although the risk of developing lymphoma has decreased in the highly active antiretroviral therapy era, this cancer remains the major cause of mortality in HIV-infected patients. Autologous hematopoietic stem cell transplantation (ASCT) outcome does not differ for HIV-infected versus HIV-uninfected patients. We propose to develop a new treatment for HIV-associated high-risk lymphoma based on autologous transplantation of two genetically modified products: CD4 T lymphocytes and CD34 hematopoietic stem cells (HSPCs). The cells will be transduced with the Cal-1 lentiviral vector encoding for both a short hairpin RNA (shRNA) against CCR5 (sh5) and the HIV-1 fusion inhibitor C46. The transduced cells will be resistant to HIV infection by two complementary mechanisms: impaired binding of the virus to the cellular CCR5 co-receptor and decreased fusion of the virus as C46 interacts with gp41 and inhibits HIV infection. This phase I/II pilot study, also entitled GENHIV, will involve two French participating centers: Saint Louis Hospital and Necker Hospital in Paris. We plan to enroll five HIV-1-infected patients presenting with high-risk lymphoma and require a treatment with ASCT. The primary objective of this study is to evaluate the safety, feasibility, and success of engraftment of Cal-1 gene-transduced CD4 T lymphocytes and CD34 HSPCs.