Link to Pubmed [PMID] – 37348801
Link to DOI – 10.1016/j.actatropica.2023.106975
Acta Trop 2023 Sep; 245(): 106975
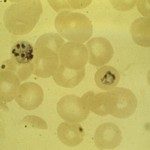
Like most countries in sub-Saharan African countries, Benin continues to bear a heavy malaria burden. In 2014, the National Malaria Control Programme (NMCP) changed its treatment policy, and recommended the use of artemisinin-based combination therapy (ACT) as first-line treatment for uncomplicated Plasmodium falciparum cases. The study presented here was conducted to investigate the impact of current antimalarial drug resistance on the country. Molecular surveillance targeting the Pfcrt, Pfmdr1, Pfkelch13, dhfr, and dhps genes was carried out on samples from patients positive for P. falciparum malaria by microscopy, LAMP and PCR diagnostic test. Molecular analysis was performed using targeted amplicon deep sequencing (TADS). In addition, the frequency of parasites with dual deletion of the histidine-rich protein 2 and 3 genes (pfhrp2 and pfhrp3), known to be responsible of the performance of HRP-based malaria rapid diagnostic tests (HRP-RDT), was estimated. Fifty-three falciparum samples collected at the Saint Jean de Dieu hospital in Tanguiéta, Benin, were tested. No Pfkelch13 validated or candidate artemisinin partial resistant variants were identified. A marked prevalence of Asn51Ile (N51I), Cys59Arg (C59R), and Ser108Asn (S108N) mutant alleles was found in the dhfr gene, representing the most frequent genotype (64%). Five-point mutations were detected in dhps, Ile431Val (I431V), Ser436Ala (S436A), Ala437Gly (A437G), Ala581Gly (A581G), Ala613Ser (A613S) of which the third was the most common (92%). No mutation was identified in dhps Lys540Glu (K540E). The quintuple mutant genotype resulting from the combination of the dhfr triple mutant (51I/59R/108N) with the dhps double mutant 436A/437G was detected at a frequency of 30%. Low levels of mutations in Pfcrt and no mutation at codon 86 in the Pfmdr1 DNA fragment were observed, whereas a high level of Tyr184Phe (Y184F) polymorphism in the Pfmdr1 gene was found. These results could be indicative, over a decade after the implementation of ACT therapy, of the return of chloroquine-sensitive but artemether-lumefantrine resistant falciparum genotypes in Benin. There was no evidence of HRP2 and HRP3 deletions. Data from the present study support the need for routine monitoring of molecular markers of antimalarial drug resistance as part of surveillance activities aimed to make informed treatment policy decisions at the national level.