Link to Pubmed [PMID] – 16160157
J. Virol. 2005 Oct;79(19):12304-10
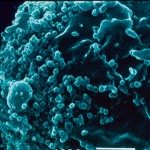
Cells constituting the placental barrier secrete soluble factors that may participate in controlling human immunodeficiency virus type 1 (HIV-1) transmission from the mother to the fetus. In this study, we asked whether placental soluble factors (PSF) could limit cell-cell contact inducing HIV-1 production that occurs after inoculation of HIV-1-infected peripheral blood mononuclear cells (HIV-1+ PBMCs) onto trophoblast-derived BeWo cells grown as tight and polarized barriers in a two-chamber system. The activity of recombinant chemokines and cytokines expressed by placental tissue and of factors secreted by either early or term placentae of HIV-1-negative women, was analyzed. We identified chemokines (RANTES and MIP-1beta) and cytokines (tumor necrosis factor alpha and interleukin-8) that decreased and increased, respectively, viral production in trophoblast barrier cells inoculated with HIV-1+ PBMCs. Unexpectedly, factors secreted by either early or term placentae of HIV-1-negative women enhanced viral production. Nevertheless, the same PSF did not favor infection of trophoblastic barriers with cell-free HIV-1 and strongly reduced viral production in PBMCs infected with cell-free HIV-1. Moreover, PSF contained chemokines (RANTES and MIP-1beta) and a cytokine, leukemia inhibitory factor, exhibiting a strong anti-HIV-1 activity in our model of cell-to-cell infection. Together these data suggested that at the maternal interface the global activity of PSF is related to the synergistic action of several soluble factors with a balance in favor of an enhancing activity on the passage of viruses across the trophoblast barrier. This could explain the presence of viral sequences in trophoblasts in all placentae of HIV-1-infected women.