About
Gerald Spaeth, PI and co-coordinator
Narissara Jariyapan (Chulalongkorn University, Bangkok, Thailand), PI and co-coordinator
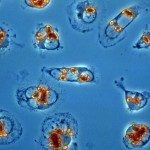
Leishmaniasis in humans is caused by at least 21 species of Leishmania parasites via sand fly bites. Infection results in three major forms of disease: cutaneous leishmaniasis (CL); mucocutaneous leishmaniasis (MCL); and visceral leishmaniasis (VL), with about 0.9-1.3 million new cases and 20,000-30,000 deaths being reported annually (Akhoundi et al. 2017; WHO 2019). The appearance of leishmaniasis in Thailand has raised an important concern that there is already a much higher underlying rate of infection than the number of clinically and parasitologically confirmed cases (about 25), for example, in a recent study a prevalence of 25.1% was indicated in HIV patients in southern Thailand (Manomat et al. 2017).
Two new species, Leishmania (Mundinia) martiniquensis and Leishmania (Mundinia) orientalis, are causative agents of leishmaniasis among Thai patients. L. martiniquensis is the most frequent cause of leishmaniasis in Thailand (Jariyapan et al. 2018). Thai research team has reported the first case of autochthonous visceral leishmaniasis in northern Thailand and the aetiological agent has been identified as L. martiniquensis (Pothirat et al. 2014). L. martiniquensis can show a range of clinical presentations, but most frequently causes VL in patients with no known underlying immunodeficiency (Pothirat et al. 2014). However, when accompanied by HIV-infection, both visceral and/or disseminated cutaneous leishmaniasis (DCL) have been reported (Chusri et al. 2012), similar to elsewhere (Chiewchanvit et al. 2015). For another species, the Thai team has also reported a case of simple cutaneous leishmaniasis diagnosed in a patient from Nan Province, Thailand. Molecular analysis of parasites derived from a biopsy sample revealed this to be a new species of Leishmania (genus Leishmania Ross, 1908), which has been named Leishmania (Mundinia) orientalis Bates & Jariyapan n. sp. (Jariyapan et al. 2018). The discovery of these unusual, pathogenic Leishmania species raises important questions on (i) their level of genetic heterogeneity and geographic adaptation, (ii) their evolutionary history compared to other more common Leishmania species endemic in Asia, and (iii) their susceptibility to current drugs and drug candidates under development. Our proposal will answer these important unsolved questions by combining the unique expertise of the Thai partner in epidemiology and clinical of L. (Mundinia) martiniquensis and L. (Mundinia) orientalis with the expertise of the French partner in comparative genomics, molecular parasitology and drug discovery.