Link to Pubmed [PMID] – 23359320
PLoS Pathog. 2013 Jan;9(1):e1003139
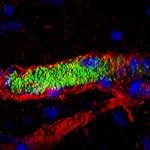
Septic shock caused by Neisseria meningitidis is typically rapidly evolving and often fatal despite antibiotic therapy. Further understanding of the mechanisms underlying the disease is necessary to reduce fatality rates. Postmortem samples from the characteristic purpuric rashes of the infection show bacterial aggregates in close association with microvessel endothelium but the species specificity of N. meningitidis has previously hindered the development of an in vivo model to study the role of adhesion on disease progression. Here we introduced human dermal microvessels into SCID/Beige mice by xenografting human skin. Bacteria injected intravenously exclusively associated with the human vessel endothelium in the skin graft. Infection was accompanied by a potent inflammatory response with the secretion of human inflammatory cytokines and recruitment of inflammatory cells. Importantly, infection also led to local vascular damage with hemostasis, thrombosis, vascular leakage and finally purpura in the grafted skin, replicating the clinical presentation for the first time in an animal model. The adhesive properties of the type IV pili of N. meningitidis were found to be the main mediator of association with the dermal microvessels in vivo. Bacterial mutants with altered type IV pili function also did not trigger inflammation or lead to vascular damage. This work demonstrates that local type IV pili mediated adhesion of N. meningitidis to the vascular wall, as opposed to circulating bacteria, determines vascular dysfunction in meningococcemia.