Link to Pubmed [PMID] – 21798616
Immunobiology 2012 May;217(5):548-57
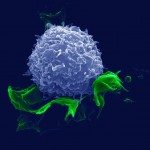
High-dose niacin therapy in humans reduces mortality from cardiovascular disease and may also protect against death from other causes, with benefits apparent more than a decade beyond the therapeutic period. Niacin therapy modulates circulating lipids, raising HDL and lowering LDL, but has the unwanted side effect of inducing skin flushing in response to treatment. Skin flushing results from niacin-induced activation of GPR109A and subsequent release of prostaglandins that promote vasodilation. GPR109A may also mediate HDL elevation. Recent data suggest that high-dose niacin may have benefits beyond improved lipid profiles, such as quelling inflammation, suggesting a potential role in immune cell trafficking. To explore effects of niacin on immune cell trafficking independently of its effects on lipid profiles, we took advantage of the fact that niacin therapy does not raise HDL in wild-type or apoE⁻/⁻ mouse strains. Wild-type and apoE⁻/⁻ C57BL/6 mice were fed standard chow or high-fat diets supplemented or not with 1% niacin. Against our predictions, this treatment did not modulate monocyte recruitment to or retention within atherosclerotic plaques. By contrast, stimulating the skin of niacin-treated mice with a contact sensitizer revealed impaired dendritic cell accumulation in draining lymph nodes and associated impaired adaptive immunity. Surprisingly, niacin-mediated impaired dendritic cell mobilization could not be reversed by cyclooxygenase inhibitor treatment nor deletion of the niacin receptor GPR109A, suggesting that the effects of niacin on modulating the migration of dendritic cells are not directly linked to skin flushing. Overall, these data suggest the existence of novel pathways triggered by niacin that, through suppression of dendritic cell migration, might impact adaptive immune responses that participate in sustained therapeutic benefits independent of niacin’s cardioprotective capabilities.