About
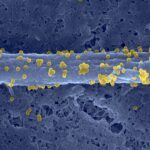
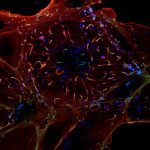
Infections of the central nervous system (CNS) are frequently severe, lethal or leading to long-term neurological sequelae. Neonates endure the highest rates of mortality and disabilities from these infections. The mechanisms responsible for the severe outcome of brain infections remain elusive, and their identification requires the use of well-characterized and representative neuroinvasive pathogens. Listeria monocytogenes (Lm) is a model bacterium, responsible for a CNS infection called neurolisteriosis, which leaves half of the surviving patients with long-term neurological impairments. In neonates, preliminary data from a nationwide cohort show that neurolisteriosis is associated with long-term severe neuropsychological defects. Our preliminary data show that Lm induces the death of brain resident macrophages, called microglia, in a mouse model of neurolisteriosis. Whereas at steady-state monocytes never contribute to microglia renewal, in mice treated to recover from infection, monocytes-derived cells replace dead microglia. Since microglia are key regulators of brain wiring and neuronal homeostasis, we hypothesize that their depletion during neurolisteriosis and replacement by monocytes may affect microglial housekeeping functions, thereby contributing to post-infectious neurodevelopmental and cognitive sequelae. To address these questions, we will first assess the dynamics and alterations in brain immune landscape during and after infection in mouse models of neonatal as well as adult neurolisteriosis, combining fate-mapping mouse lines and single-cell transcriptomics approaches. We will then assess the neuronal alterations induced by microglia depletion and replacement, as well as the long-term cognitive impact on previously infected mice. This project will highlight how altering brain immune cells during infection can be responsible for neurological impairments, and may help in identifying therapeutic approaches to treat such sequelae.