Lien vers Pubmed [PMID] – 39213164
Lien DOI – 10.1128/jvi.01113-24
J Virol 2024 Aug; (): e0111324
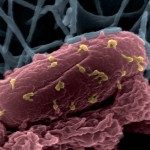
Bacteria exposed to bactericidal treatment, such as antibiotics or bacteriophages (phages), often develop resistance. While phage therapy is proposed as a solution to the antibiotic resistance crisis, the bacterial resistance emerging during phage therapy remains poorly characterized. In this study, we examined a large population of phage-resistant extra-intestinal pathogenic Escherichia coli 536 clones that emerged from both in vitro (non-limited liquid medium) and in vivo (murine pneumonia) conditions. Genome sequencing uncovered a convergent mutational pattern in phage resistance mechanisms under both conditions, particularly targeting two cell-wall components, the K15 capsule and the lipopolysaccharide (LPS). This suggests that their identification in vivo could be predicted from in vitro assays. Phage-resistant clones exhibited a wide range of fitness according to in vitro tests, growth rate, and resistance to amoeba grazing, which could not distinguish between the K15 capsule and LPS mutants. In contrast, K15 capsule mutants retained virulence comparable to the wild-type strain, whereas LPS mutants showed significant attenuation in the murine pneumonia model. Additionally, we observed that resistance to the therapeutic phage through a nonspecific mechanism, such as capsule overproduction, did not systematically lead to co-resistance to other phages that were initially capable or incapable of infecting the wild-type strain. Our findings highlight the importance of incorporating a diverse range of phages in the design of therapeutic cocktails to target potential future phage-resistant clones effectively.This study isolated more than 50 phage-resistant mutants from both in vitro and in vivo conditions, exposing an extra-intestinal pathogenic Escherichia coli strain to a single virulent phage. The characterization of these clones revealed several key findings: (1) mutations occurring during phage treatment affect the same pathways as those identified in vitro; (2) the resistance mechanisms are associated with the modification of two cell-wall components, with one involving receptor deletion (phage-specific mechanism) and the other, less frequent, involving receptor masking (phage-nonspecific mechanism); (3) an in vivo virulence assay demonstrated that the absence of the receptor abolishes virulence while masking the receptor preserves it; and (4) clones with a resistance mechanism nonspecific to a particular phage can remain susceptible to other phages. This supports the idea of incorporating diverse phages into therapeutic cocktails designed to collectively target both wild-type and phage-resistant strains, including those with resistance mechanisms nonspecific to a phage.