Lien vers Pubmed [PMID] – 20089698
J. Immunol. 2010 Feb;184(4):2076-85
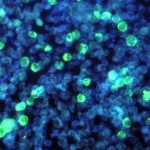
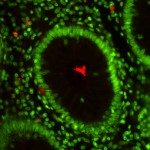
The T cell response to Shigella, the causative agent of bacillary dysentery, remains poorly understood. Using a murine model of infection, we report that Shigella flexneri primes predominately IL-17A- and IL-22-producing Th17 cells. Shigella-specific Th1 cells are only significantly induced on secondary infection, whereas specific Th2 and CD8(+) T cells are undetectable. Apart from Th17 cells that are primed in a MHC class II- and IL-6-dependent, but IL12/23p40-independent manner, we identified gammadelta T cells as an additional but minor source of IL-17A. Priming of IL-17A(+) gammadelta T cells is dependent on IL12/23p40, but independent of MHC-class II and IL-6. Th17 cells have emerged as important players in inflammatory, autoimmune, and infectious diseases. Among the yet unresolved questions is their role in long-term immunity to pathogens. In this study, we show that the elicited S. flexneri-specific Th17 pool gives rise to an enhanced recall response up to 12 mo after priming, suggesting the presence of a long-term memory state. The clearance of primary infection is impaired in the absence of T cells, but independently of IL-17A. However, after reinfection, IL-17A produced by S. flexneri-specific Th17 cells becomes important to ultimately restrict bacterial growth. These findings bring new insights into the adaptive immune response to Shigella infection and highlight the importance of pathogen-specific Th17 cell immunity for secondary immune protection.