Lien vers Pubmed [PMID] – 31182526
Antimicrob. Agents Chemother. 2019 Aug;63(8)
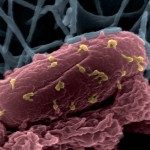
Supported by years of clinical use in some countries and more recently by literature on experimental models, as well as its compassionate use in Europe and in the United States, bacteriophage (phage) therapy is providing a solution for difficult-to-treat bacterial infections. However, studies of the impact of such treatments on the host remain scarce. Murine acute pneumonia initiated by intranasal instillation of two pathogenic strains of (536 and LM33) was treated by two specific bacteriophages (536_P1 and LM33_P1; intranasal) or antibiotics (ceftriaxone, cefoxitin, or imipenem-cilastatin; intraperitoneal). Healthy mice also received phages alone. The severity of pulmonary edema, acute inflammatory cytokine concentration (blood and lung homogenates), complete blood counts, and bacterial and bacteriophage counts were determined at early (≤12 h) and late (≥20 h) time points. The efficacy of bacteriophage to decrease bacterial load was faster than with antibiotics, but the two displayed similar endpoints. Bacteriophage treatment was not associated with overinflammation but in contrast tended to lower inflammation and provided a faster correction of blood cell count abnormalities than did antibiotics. In the absence of bacterial infection, bacteriophage 536_P1 promoted a weak increase in the production of antiviral cytokines (gamma interferon [IFN-γ] and interleukin-12 [IL-12]) and chemokines in the lungs but not in the blood. However, such variations were no longer observed when bacteriophage 536_P1 was administered to treat infected animals. The rapid lysis of bacteria by bacteriophages does not increase the innate inflammatory response compared to that with antibiotic treatment.