Lien vers Pubmed [PMID] – 24103142
Transpl Infect Dis 2013 Dec;15(6):E235-8
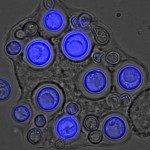
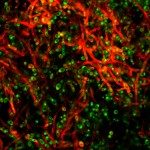
Mucormycosis, an emerging fungal infection in solid organ transplant patients, is mostly located in rhino-orbito-cerebral, pulmonary, and cutaneous areas, or disseminated with poor prognosis. A 4-year-old girl with chronic intestinal pseudo-obstruction syndrome underwent a modified multivisceral transplantation, including half of the stomach, the duodeno-pancreas, the small bowel, and the right colon. On postoperative day 5, a digestive perforation was suspected. Surgical exploration found a small necrotic area on the native stomach, which was externally drained. The next day, massive gastric bleeding occurred. During the emergency laparotomy, 2 hemorrhagic ulcers were found and resected from the transplanted stomach. Pathology and fungal culture showed mucormycosis caused by Lichtheimia (formerly Absidia) ramosa in both the transplanted and native stomach. High-dose intravenous liposomal amphotericin B was immediately started. No other site of fungal infection was found. The child recovered, and 3 years after transplantation, is alive and well, off parenteral nutrition. The originality of this case is the very early presentation after transplantation, the unusual site, and the complete recovery after rapid medico-surgical management. The origin of the fungus and treatment are discussed.