Lien vers Pubmed [PMID] – 28973855
Proc. Natl. Acad. Sci. U.S.A. 2017 Oct;114(41):E8675-E8684
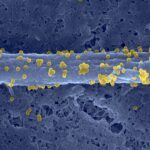
It has been known for some time that atherosclerotic lesions preferentially develop in areas exposed to low SS and are characterized by a proinflammatory, apoptotic, and senescent endothelial phenotype. Conversely, areas exposed to high SS are protected from plaque development, but the mechanisms have remained elusive. Autophagy is a protective mechanism that allows recycling of defective organelles and proteins to maintain cellular homeostasis. We aimed to understand the role of endothelial autophagy in the atheroprotective effect of high SS. Atheroprotective high SS stimulated endothelial autophagic flux in human and murine arteries. On the contrary, endothelial cells exposed to atheroprone low SS were characterized by inefficient autophagy as a result of mammalian target of rapamycin (mTOR) activation, AMPKα inhibition, and blockade of the autophagic flux. In hypercholesterolemic mice, deficiency in endothelial autophagy increased plaque burden only in the atheroresistant areas exposed to high SS; plaque size was unchanged in atheroprone areas, in which endothelial autophagy flux is already blocked. In cultured cells and in transgenic mice, deficiency in endothelial autophagy was characterized by defects in endothelial alignment with flow direction, a hallmark of endothelial cell health. This effect was associated with an increase in endothelial apoptosis and senescence in high-SS regions. Deficiency in endothelial autophagy also increased TNF-α-induced inflammation under high-SS conditions and decreased expression of the antiinflammatory factor KLF-2. Altogether, these results show that adequate endothelial autophagic flux under high SS limits atherosclerotic plaque formation by preventing endothelial apoptosis, senescence, and inflammation.