Présentation
Healthcare-associated infections are caused by a diversity of pathogenic micro-organisms, which together represent leading causes of global infectious disease morbidity and mortality. The objective of this thesis was to develop novel mathematical models to evaluate the transmission dynamics of antibiotic-resistant bacteria and SARS-CoV-2 in healthcare settings, and to provide evidence for the design and optimization of species-specific surveillance and control interventions.
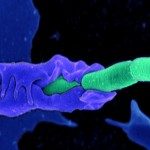
First, a modelling framework for the hospital epidemiology of antibiotic-resistant bacteria was formalized. This framework accounts for within-host mechanisms of ecological interaction between the host microbiome and bacterial pathogens in the context of antibiotic exposure. Microbiome-pathogen interactions, including microbiome-induced colonization resistance and the interspecific horizontal transfer of antibiotic resistance genes, were found to underlie trade-offs in how antibiotics select for the epidemiological spread of resistance. In a simulation study using this framework, contact precautions were effective for prevention of colonization with methicillin-resistant Staphylococcus aureus but not multidrug-resistant Enterobacteriaceae, while antibiotic stewardship interventions and microbiome-targeted therapies were broadly effective across species.
Second, simulations from an individual-based SARS-CoV-2 transmission model were used to inform optimization of testing and screening interventions in long-term care facilities. In an early pandemic context, group testing (sample pooling) was the most efficient means to detect emerging outbreaks in resource-limited facilities, while hierarchical testing cascades were most effective given high testing capacity. In a later pandemic context, population screening using rapid antigen diagnostic testing was an effective but time-sensitive means to prevent nosocomial transmission.
Overall, work from this thesis represents a first step in understanding how the microbiome influences nosocomial transmission risk of antibiotic resistance, and provides evidence for optimizing SARS-CoV-2 surveillance in the context of limited and imperfect testing resources.