Link to Pubmed [PMID] – 27122576
J. Virol. 2016 Apr; 90(13):6148-58
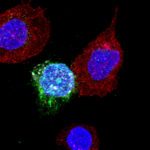
HIV establishes reservoirs of infected cells that persist despite effective antiretroviral therapy (ART). In most patients, the virus begins to replicate soon after treatment interruption. However, a low frequency of infected cells at the time of treatment interruption has been associated with delayed viral rebound. Likewise, individuals who control the infection spontaneously, so-called “HIV-1 controllers” (HICs) carry particularly low levels of infected cells. It is unclear, however, whether and how this small number of infected cells contributes to durable viral control. Here we compared 38 HICs with 12 patients on effective combined ART (“cART patients”) and found that the low frequency of infected cells in the former subjects was associated both with less efficient viral reactivation in resting CD4+ T cells and with less efficient virion production ex vivo We also found that a potent HIV-specific CD8+ T cell response was only present in those HICs whose CD4+ T cells produced virus ex vivo. Long-term spontaneous control of HIV infection in HICs thus appears to be sustained on the inefficient reactivation of viruses from a limited number of infected cells, and the capacity of HICs to activate a potent HIV-specific CD8+ T cell response to counteract efficient viral reactivation events.
IMPORTANCE: There is a strong scientific interest in developing strategies to eradicate the HIV-1 reservoir. Very rare HIV-1 infected patients are able to spontaneously control viremia for long periods of time (HIV-1 controllers, HIC) and are put forward as a model of HIV-1 remission. Here, we show that the low viral reservoirs found in HIC are a critical part of the mechanisms underlying viral control and traduces in a lower probability of HIV-1 reactivation events resulting in limited HIV-1 release and spread. We found that those HIC in whom viral reactivation and spread in vitro from CD4+ T cells was most difficult were those with shrunk CD8+ T cell responses. These results suggest that low HIV-1 reservoirs, in some settings, decisively contribute to at least temporary control of infection without antiretroviral therapy. We believe that this work provides information of relevance in the context of the search for HIV-1 remission.