According to a study published in Nature Climate Change (2022), 58% of infectious or allergic diseases have already been aggravated by climate-related hazards. The World Health Organization (WHO) estimates that between 2030 and 2050, climate change could cause an additional 250,000 deaths per year from malnutrition, malaria, diarrhea, and heatwaves, with an economic impact of €2–4 billion annually.
By disrupting ecosystems and increasing human-wildlife interactions, environmental changes also facilitate the emergence of novel pathogens. Viruses such as HIV, Nipah, Ebola, COVID-19, and Mpox exemplify how anthropogenic pressures on natural habitats can trigger zoonotic spillovers.
Environmental transitions, including climate change, ecological shifts, pollution, and urbanization, are increasingly shaping human health. Changes in temperature, precipitation, and land use modify the distribution of pathogens and vectors, contributing to the emergence and spread of infectious diseases such as malaria, dengue, Zika, and Lyme disease. In addition, environmental stressors exacerbate non-communicable and inflammatory diseases, including cardiovascular diseases, respiratory conditions, metabolic disorders, and certain cancers.
Pasteur 2030 Strategy
Through European and global partnerships, the Institut Pasteur investigates how environmental and climatic factors drive pathogen emergence and vector dynamics. Collaborative efforts also develop innovative tools for early detection, surveillance, and outbreak modeling — positioning Pasteur 2030 as a leader in understanding and mitigating the health impacts of environmental transitions.
1. Understanding Environmental Drivers of Disease
Pasteur 2030 aims to unravel how climate change and ecological transitions drive the emergence and spread of infectious and non-communicable diseases. This includes mechanistic studies on vector-pathogen-host interactions, the influence of temperature, humidity, and urbanization on vector distribution, and modeling of environmental risk factors.
2. Advancing Early Detection and Epidemic Intelligence
The Institute strengthens epidemic intelligence by integrating field surveillance, National Reference Centers, the Biological Emergency Response Unit (CIBU), and pathogen discovery laboratories. Early detection, sample collection, and rapid data analysis enable timely modeling of epidemic dynamics and proactive intervention strategies.
3. Developing Targeted Countermeasures
Building on mechanistic insights, Pasteur develops novel diagnostics, vaccines, and therapeutics. This includes identifying molecular targets, designing rapid diagnostic tests for emerging pathogens, and testing interventions in collaboration with academic, industrial, and hospital partners. The Institute also evaluates susceptibility factors such as genetics, immunity, and microbiota to inform preventive strategies.
Flagship Projects
Center for Infection, Climate and Environment (ICE)
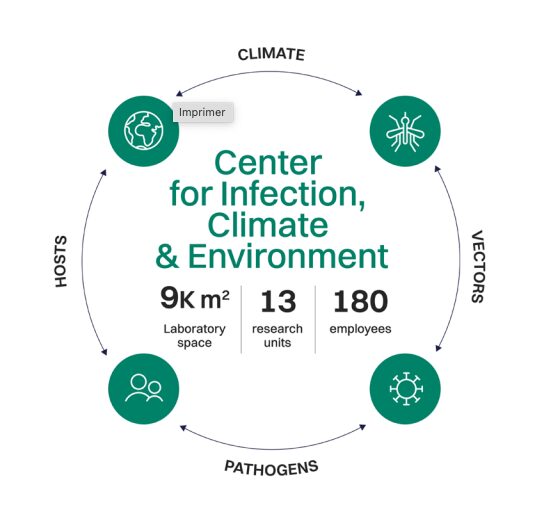
Opening in 2028, the ICE will host cutting-edge Biosafety Level 3 facilities dedicated to vector-borne and environmentally emerging pathogens. Research will focus on pathogen–vector–host interactions using advanced imaging and modeling, while fostering global collaboration and training in a secure, state-of-the-art environment.
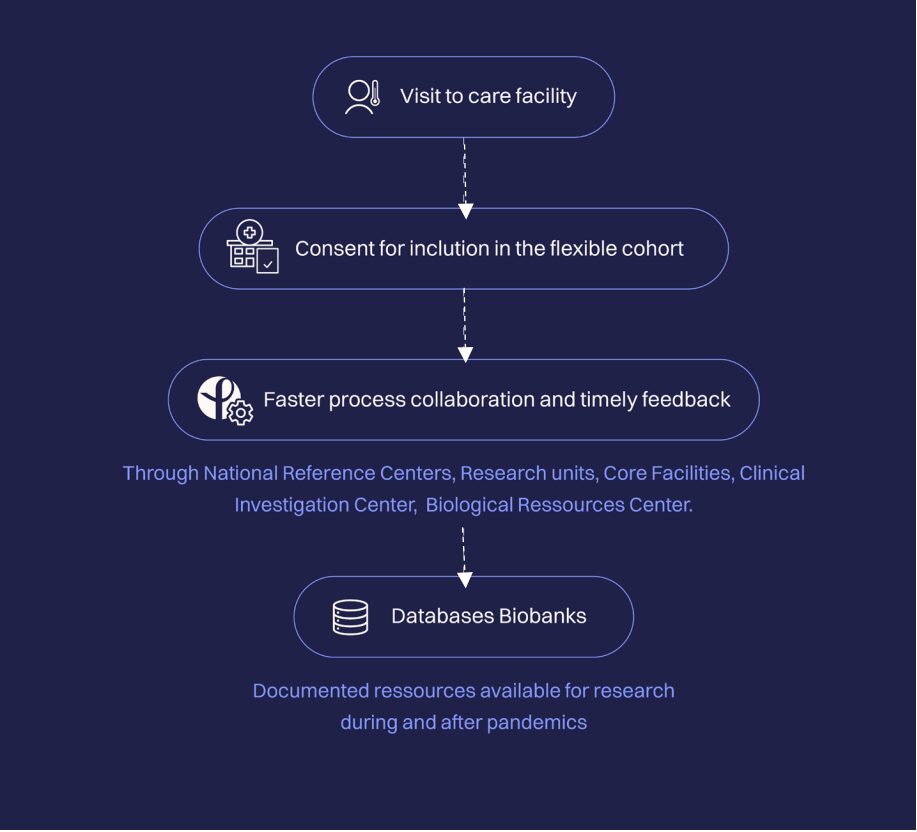
Pasteur Pandemics Preparedness Initiative (P3I)
P3I strengthens pandemic preparedness by deepening knowledge of pathogens, accelerating countermeasure development, enhancing surveillance, and supporting rapid outbreak responses through the Outbreak Investigation Task Force (OITF). It also establishes flexible cohorts for real-time data sharing and research deployment.
Both initiatives align with key partners — ANSES, Inserm, AP-HP, Inrae, and the Pasteur Network — promoting a comprehensive One Health approach that integrates human, animal, and environmental health.





