Lien vers Pubmed [PMID] – 23924269
Am. J. Respir. Crit. Care Med. 2013 Sep;188(6):684-92
RATIONALE: Purpura fulminans in adults is a rare but devastating disease. Its pathophysiology is not well known.
OBJECTIVES: To understand the pathophysiology of skin lesions in purpura fulminans, the interplay between circulating blood and vascular alterations was assessed.
METHODS: Prospective multicenter study in four intensive care units. Patients with severe sepsis without skin lesions were recruited as control subjects.
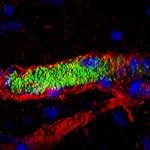
MEASUREMENTS AND MAIN RESULTS: Twenty patients with severe sepsis and purpura fulminans were recruited for blood sampling, and skin biopsy was performed in deceased patients. High severity of disease and mortality rates (80%) was observed. Skin biopsies in purpura fulminans lesions revealed thrombosis and extensive vascular damage: vascular congestion and dilation, endothelial necrosis, alteration of markers of endothelial integrity (CD31) and of the protein C pathway receptors (endothelial protein C receptor, thrombomodulin). Elevated plasminogen activating inhibitor-1 mRNA was also observed. Comparison with control patients showed that these lesions were specific to purpura fulminans. By contrast, no difference was observed for blood hemostasis parameters, including soluble thrombomodulin, activated protein C, and disseminated intravascular coagulation markers. Bacterial presence at the vascular wall was observed specifically in areas of vascular damage in eight of nine patients tested (including patients with Streptococcus pneumoniae, Neisseria meningitidis, Escherichia coli, and Pseudomonas aeruginosa infection).
CONCLUSIONS: Thrombi and extensive vascular damage with multifaceted prothrombotic local imbalance are characteristics of purpura fulminans. A “vascular wall infection” hypothesis, responsible for endothelial damage and subsequent skin lesions, can be put forward.