Lien vers Pubmed [PMID] – 22247443
Clin. Infect. Dis. 2012 Feb;54 Suppl 1:S35-43
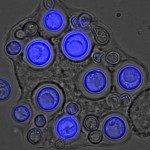
BACKGROUND: Mucormycosis is a deadly invasive fungal infection whose characteristics are only partially understood.
METHODS: Data on mucormycosis obtained in France between 2005 and 2007 from 2 notification systems were merged. The 2008 European Organisation for Research and Treatment of Cancer/Mycoses Study Group definition criteria were applied and risk factors for death were analyzed by hazard ratios (HRs) calculated from the Cox proportional hazards regression model.
RESULTS: A total of 101 cases (60 proven, 41 probable), mostly in men (58%) >50 years (mean age, 50.7 ± 19.9) were recorded. Hematological malignancies represented 50% (median time for occurrence, 8.8 months after disease onset), diabetes 23%, and trauma 18% of cases. Sites of infection were lungs (28%; 79% in hematology patients), rhinocerebral (25%; 64% in diabetic patients), skin (20%), and disseminated (18%). Median time between first symptoms and diagnosis was 2 weeks. The main fungal species were Rhizopus oryzae (32%) and Lichtheimia species (29%). In cases where the causative species was identified, R. oryzae was present in 85% of rhinocerebral forms compared with only 17% of nonrhinocerebral forms (P < .001). Treatment consisted of surgery in 59% and antifungals in 87% of cases (liposomal amphotericin B in 61%). Ninety-day survival was 56%; it was reduced in cases of dissemination compared with rhinocerebral (HR, 5.38 [2.0-14.1]; P < .001), pulmonary (HR, 2.2 [1.0-4.7]; P = .04), or skin localization (HR, 5.73 [1.9-17.5]; P = .002); survival was reduced in cases of hematological malignancies compared with diabetes mellitus (HR, 2.3 [1.0-5.2]; P < .05) or trauma (HR, 6.9 [1.6-28.6], P = .008) and if ≥2 underlying conditions (HR, 5.9 [1.8-19.0]; P = .004). Mucormycosis localization remained the only independent factor associated with survival.
CONCLUSIONS: This 3-year study performed in one country shows the diverse clinical presentation of mucormycosis with a high prevalence of primary skin infection following trauma and a prognosis significantly influenced by localization.