Link to Pubmed [PMID] – 23286863
Liver Int. 2013 Feb;33 Suppl 1:182-7
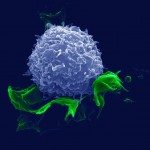
Hepatitis B virus (HBV) infection is more frequent in immune deficient populations than in the general population with lower rates of spontaneous recovery in acute cases, thus explaining the high rate of chronic infection and the increased risk of cirrhosis and hepatocellular carcinoma, resulting in increased morbidity-mortality in these patients. The negative impact of immune deficiency on chronic HBV infection is related to two non-exclusive factors: (i) high viral load enhances the progression of fibrosis and may result in a rare severe liver disease called fibrosing cholestatic hepatitis, which reflects the direct toxicity of high levels of HBV proteins; (ii) The pathobiology of HBV infection is mainly immune-mediated via HBV-specific T lymphocytotoxicity. The reduction or discontinuation of immune deficiency may result in severe liver disease including fulminant hepatitis from immune restoration. Thus, immune deficiency enhances the hepatitis B viral load, which results in the progression of fibrosis and/or acute exacerbation of underlying liver disease (HBV reactivation) on one hand, whereas reduction in immune deficiency may also be harmful because of immune restoration on the other hand. This double-edged sword explains why the diagnosis and evaluation of the impact of HBV infection on the liver must be especially rigorous in cases of immune deficiency whatever the cause: transplantation, oncology, haematology, internal medicine (rheumatology, gastroenterology …) or HIV infection, and why pre-emptive therapy by HBV nucleos(t)ide analogues should be considered for all HBV-infected patients.