Link to Pubmed [PMID] – 36157543
Link to DOI – 10.3748/wjg.v28.i29.3903
World J Gastroenterol 2022 Aug; 28(29): 3903-3916
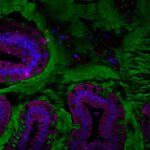
Chronic abdominal pain is the most common cause for gastroenterology consultation and is frequently associated with functional gastrointestinal disorders including irritable bowel syndrome and inflammatory bowel disease. These disorders present similar brain/gut/microbiota trialogue alterations, associated with abnormal intestinal permeability, intestinal dysbiosis and colonic hypersensitivity (CHS). Intestinal dysbiosis can alter colon homeostasis leading to abnormal activation of the innate immunity that promotes CHS, perhaps involving the toll-like receptors (TLRs), which play a central role in innate immunity.To understand the mechanisms between early life event paradigm on intestinal permeability, fecal microbiota composition and CHS development in mice with TLRs expression in colonocytes.Maternal separation model (NMS) CHS model, which mimics deleterious events in childhood that can induce a wide range of chronic disorders during adulthood were used. Colonic sensitivity of NMS mice was evaluated by colorectal distension (CRD) coupled with intracolonic pressure variation (IPV) measurement. Fecal microbiota composition was analyzed by 16S rRNA sequencing from weaning to CRD periods. TLR mRNA expression was evaluated in colonocytes. Additionally, the effect of acute intrarectal instillation of the TLR5 agonist flagellin (FliC) on CHS in adult naive wildtype mice was analyzed.Around 50% of NMS mice exhibited increased intestinal permeability and CHS associated with intestinal dysbiosis, characterized by a significant decrease of species richness, an alteration of the core fecal microbiota and a specific increased relative abundance of flagellated bacteria. Only TLR5 mRNA expression was increased in colonocytes of NMS mice with CHS. Acute intrarectal instillation of FliC induced transient increase of IPV, reflecting transient CHS appearance.Altogether, these data suggest a pathophysiological continuum between intestinal dysbiosis and CHS, with a role for TLR5.