Link to Pubmed [PMID] – 28066361
Link to DOI – 203810.3389/fmicb.2016.02038
Front Microbiol 2016 ; 7(): 2038
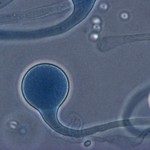
Candida glabrata is a major pathogenic yeast in humans that is known to rapidly acquire resistance to triazole and echinocandin antifungal drugs. A mutator genotype (MSH2 polymorphism) inducing a mismatch repair defect has been recently proposed to be responsible for resistance acquisition in C. glabrata clinical isolates. Our objectives were to evaluate the prevalence of antifungal resistance in a large cohort of patients in Saint-Louis hospital, Paris, France, some of whom were pre-exposed to antifungal drugs, as well as to determine whether MSH2 polymorphisms are associated with an increased rate of fluconazole or echinocandin resistance. We collected 268 isolates from 147 patients along with clinical data and previous antifungal exposure. Fluconazole and micafungin minimal inhibition concentrations (MICs) were tested, short tandem repeat genotyping was performed, and the MSH2 gene was sequenced. According to the European Committee on Antimicrobial Susceptibility breakpoints, 15.7% of isolates were resistant to fluconazole (MIC > 32 mg/L) and 0.7% were resistant to micafungin (MIC > 0.03 mg/L). A non-synonymous mutation within MSH2 occurred in 44% of the isolates, and 17% were fluconazole resistant. In comparison, fluconazole resistant isolates with no MSH2 mutation represented 15% (P = 0.65). MSH2 polymorphisms were associated with the short tandem repeat genotype. The rate of echinocandin resistance is low and correlates with prior exposure to echinocandin. The mutator genotype was not associated with enrichment in fluconazole resistance but instead corresponded to rare and specific genotypes.